
What’s the Doctor got to do with it?
Have you ever considered how much influence the relationship with your health care provider has on your health? When selecting a healthcare provider to work with, are there certain things you look for, or standards you have? Or is it merely, check the task box of things such as: they’re in network, the office is near me, and/or I can get in and see them quickly?
“By far the most frequent drug used in general practice was the doctor himself. It was not the bottle of medicine or the box of pills that mattered but the way the doctor gave them to his patient.”
-Michael Balint
Often times, especially if we do not experience many health concerns, this is not something that we put much thought or energy in considering. If you have more complex health conditions, or experience a significant health scare; you may be more motivated to do a bit more research; but just as with living a healthy lifestyle, finding a good doctor early on may be a pivotal part in health promotion and disease prevention both in the short and long-term.
Let me share a few facts on the doctor relationship, and why you might want to reconsider your healthcare experience. The average office visit with a doctor or health care provider in the United States is approximately 10-15 minutes long (1). In that visit, it is estimated that you will have 12-23 seconds to explain the intention of your visit and symptom history before the provider interrupts you, and during the entire encounter you (the patient) will have a total of 4 minutes of speaking time, with an average of 2 interruptions (2,3).
It may not be so much that office visits, are short, but it’s HOW they are used that makes all the difference. How do these factors affect health outcomes? Well let’s take a look – In a study of patients with the common cold, researchers examined three groups: standard visits, enhanced visits, or no visits at all (4). A standard visit was as described above short, and provider-centric (or less listening to the patient). Where in the “enhanced” visits the providers took more time, made eye contact, and intentionally listened to the patients complaints and concerns. Then there was the group who did not go to the doctor at all. Researchers measured the duration of illness/time to recovery from each intervention (or lack thereof) and what they found, perhaps by no surprise, is that those who received enhanced care recovered quicker than those who received conventional care. What’s most surprising is the finding that those who had standard visits; did worse than those who did not see a healthcare provider at all (4,5).
Another examined the use of “warm, emphatic interaction” against “neutral interaction” or “wait list/no visits” in patients who were suffering from irritable bowel syndrome, and the findings were consistent. Those who had an enhanced visit, where there was perceived caring and compassion, responded positively to the placebo acupuncture they received. The neutral groups, and those who received no care at all, were nearly identical in symptom response (6).
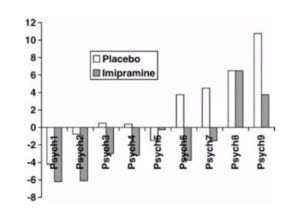
Similarly this effect was observed in those who suffered from depression. Researchers analyzed the effect of psychiatrist on patient outcomes. In their analysis, there were two groups, one received a placebo and were placed in “enhanced” therapy with psychiatrist who were present and compassionate. The second groups received antidepressant medication (Imipramine), were placed in standard therapy, and psychiatrist displayed less “connection” to the client. Both groups were followed over several weeks, and what was observed was that the placebo group not only saw a significant improvement in symptoms compared to those who received approved medication therapy, but noticed symptom improvement much earlier than those receiving standard therapy.
Concluding remarks of the study: “..it can be concluded that effective psychiatrists can, in fact, augment the effects of the active ingredients of anti-depressant medication as well as placebo… and psychiatrist effects were greater than the treatment” in this study (7).
“One of the first duties of the physician is to educate the masses not to take medicine.”
-Sir William Osler
These studies are just a few of the many that demonstrate not only the power of the mind and the dynamic variables of healing, but the importance and power of the therapeutic interaction between humans.
With this insight, take some time to reflect on your relationship with your healthcare provider, and consider how you might shift your checkbox of requirements from convenience factors to factors that invest in your health. If you find that your new standards aren’t being met, consider using this new framework and criteria to seek out a better fit for you and your health goals.
Characteristics and Requirements of a therapeutic relationship:
- An emotionally charged RELATIONSHIP (versus interaction) with a helping person.
- Deep listening and presence
- Compassion
- Trust
- A healing setting (A place to go for healing), that does not feel pressured or rushed.
- An EXPLANATION for symptoms, rather than just a diagnosis. (the WHY behind condition/experience)
- Therapy and interventions that address the ROOT CAUSE of disease/dysfunction.
- Consideration and respect for individual preferences.
- Openness and accommodation to individual needs and preferences.
- Awareness of what is the most meaningful and motivating health goal for the individual.
- A ritual, procedure, or plan that involves active participation of both patient and provider, that each believes will restore the person to a state of health.
- Ability to “meet in the middle” and open to challenging fixed beliefs upon what is best for all, but what is best for each individual.
- Utilization of up-to-date current science of health (within their specific area of practice). Actively participating in continuing education and learning.
- Ongoing evolution of plan of care based upon changes in health and most recent science.
At VSMG, we are committed to educating, supporting, and encouraging programs for our members that help each person live their best lives and have a strong relationship with their doctor. Finding and fostering the right relationship with your physician is just one way we can help our members get and stay healthy!
References.Sinsky, C., Colligan, L., Li, L., Prgomet, M., Reynolds, S., Goeders, L., … & Blike, G. (2016). Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Annals of internal medicine, 165(11), 753-760.
Rhodes, D. R., McFarland, K. F., Finch, W. H., & Johnson, A. O. (2001). Speaking and interruptions during primary care office visits. FAMILY MEDICINE-KANSAS CITY-, 33(7), 528-532.Marvel, M. K., Epstein, R. M., Flowers, K., & Beckman, H. B. (1999). Soliciting the patient’s agenda: have we improved?. Jama, 281(3), 283-287.
Rakel, D. P., Hoeft, T. J., Barrett, B. P., Chewning, B. A., Craig, B. M., & Niu, M. (2009). Practitioner empathy and the duration of the common cold. Family medicine, 41(7), 494.Rakel, D., Barrett, B., Zhang, Z., Hoeft, T., Chewning, B., Marchand, L., & Scheder, J. (2011). Perception of empathy in the therapeutic encounter: effects on the common cold. Patient education and counseling, 85(3), 390-397.
Kelley, J. M., Lembo, A. J., Ablon, J. S., Villanueva, J. J., Conboy, L. A., Levy, R., … Kaptchuk, T. J. (2009). Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosomatic medicine, 71(7), 789–797. doi:10.1097/PSY.0b013e3181acee12McKay, K. M., Imel, Z. E., & Wampold, B. E. (2006). Psychiatrist effects in the psychopharmacological treatment of depression. Journal of affective disorders, 92(2-3), 287-290.



